Who gets heart disease?
Heart disease can affect people of all ages, genders, and backgrounds. However, there are certain factors that can increase the risk of developing heart disease. Some common risk factors include:
- Age: The risk of heart disease increases with age. Men over 45 and women over 55 are more likely to develop heart disease.
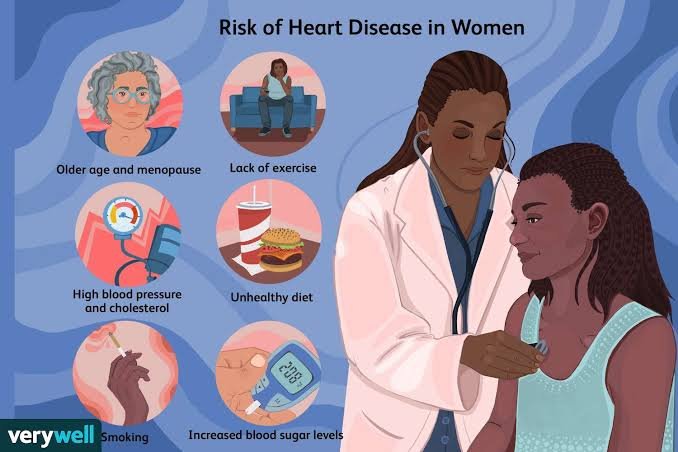
- Gender: Men have a higher risk of heart disease than premenopausal women. However, after menopause, a woman’s risk increases and becomes similar to that of men.
- Family history: Having a close family member, such as a parent or sibling, with heart disease increases your risk.
- Smoking: Smoking damages the blood vessels and can lead to the development of heart disease.
- High blood pressure: Hypertension puts strain on the heart and increases the risk of heart disease.
- High cholesterol levels: Elevated levels of LDL (bad) cholesterol and triglycerides can contribute to the formation of plaques in the arteries, leading to heart disease.
- Obesity and overweight: Excess weight, especially around the waist, increases the risk of heart disease.
- Diabetes: People with diabetes have an increased risk of developing heart disease due to elevated blood sugar levels damaging blood vessels and nerves.
- Sedentary lifestyle: Lack of regular physical activity can contribute to the development of heart disease.
- Unhealthy diet: A diet high in saturated and trans fats, cholesterol, salt, and sugar can increase the risk of heart disease.
It’s important to note that while these risk factors increase the likelihood of developing heart disease, they do not guarantee its occurrence. Adopting a healthy lifestyle, managing risk factors, and seeking regular medical check-ups can help reduce the risk and promote heart health.
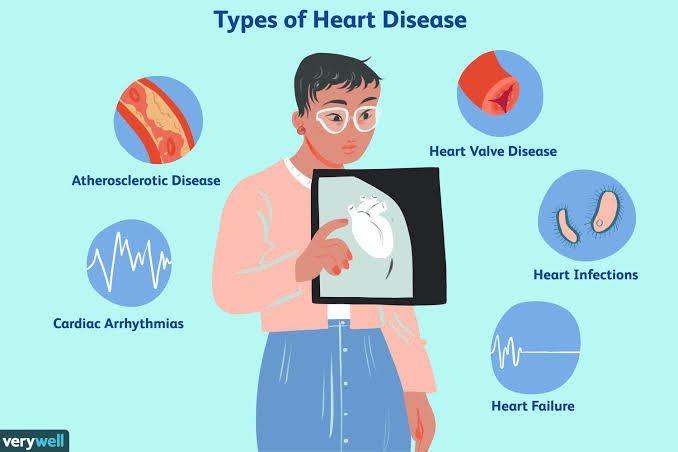
What are the different types of heart disease?
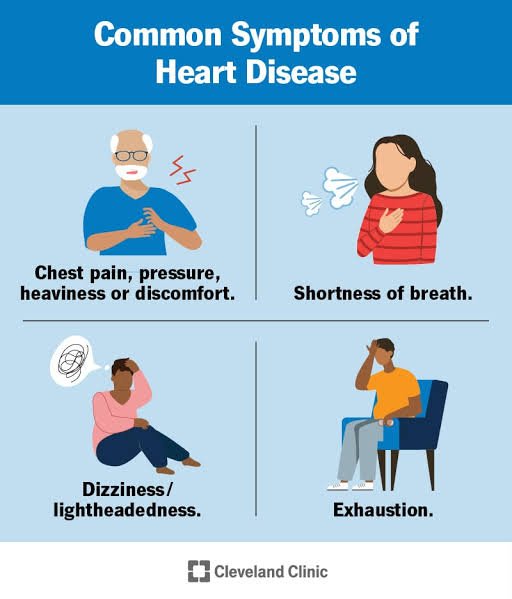
The symptoms of heart disease can vary depending on the specific condition and its severity. Here are some common symptoms associated with various types of heart disease:
- Chest pain or discomfort: This is a classic symptom of coronary artery disease. It may manifest as pressure, tightness, squeezing, or a burning sensation in the chest (angina). The pain may also radiate to the arms, shoulders, neck, jaw, or back.
- Shortness of breath: Feeling breathless or having difficulty breathing, especially during physical activity or while lying flat, can be a sign of heart failure, coronary artery disease, or heart valve problems.
- Fatigue: Unexplained or excessive fatigue, weakness, or a decreased ability to perform regular activities can be a symptom of heart disease. The heart’s reduced pumping efficiency can result in inadequate oxygen supply to the body’s tissues.
- Rapid or irregular heartbeat: Heart palpitations, a sensation of a racing or irregular heartbeat, can occur with arrhythmias. This may be accompanied by lightheadedness, dizziness, or fainting.
- Swelling: Fluid retention can lead to swelling in the feet, ankles, legs, abdomen, or even the veins in the neck. It can be a sign of heart failure or other heart-related issues.
- Dizziness or fainting: Reduced blood flow to the brain due to a heart problem can cause feelings of lightheadedness, dizziness, or fainting (syncope).
- Nausea and vomiting: Some people with heart disease may experience nausea, indigestion, or vomiting, which can be mistaken for gastrointestinal issues.
- Cold sweats: Profuse sweating with clammy skin, particularly when accompanied by other symptoms like chest pain or shortness of breath, may indicate a heart attack.
It’s important to note that these symptoms can also be associated with other conditions, and some individuals with heart disease may not experience any noticeable symptoms. If you have concerns about heart disease or are experiencing any of these symptoms, it’s essential to seek medical attention for a proper evaluation and diagnosis.
What are the symptoms of heart disease?
Heart disease can present differently in women compared to men. Women may experience some of the same symptoms as men, but there are also specific symptoms that are more commonly observed in women. Here are some symptoms of heart disease that are frequently reported by women:
- Chest discomfort: Women may experience chest pain or discomfort that is different from the typical “crushing” or “squeezing” chest pain often associated with a heart attack in men. Women may describe it as a sharp, burning, or stabbing pain in the chest.
- Shortness of breath: Breathlessness, difficulty breathing, or feeling winded, especially during physical exertion or even during rest, can be a symptom of heart disease in women.
- Fatigue: Unexplained or excessive fatigue and weakness can be signs of heart disease in women. Fatigue may occur even with minimal physical activity and can interfere with daily tasks.
- Pain in the neck, jaw, throat, or upper abdomen: Women may experience pain or discomfort in areas other than the chest during a heart attack. This pain can radiate from the chest to these areas or can occur without chest pain.
- Back pain: Some women may experience pain or discomfort in the back, particularly between the shoulder blades, during a heart attack.
- Nausea, vomiting, or indigestion: Women may experience gastrointestinal symptoms such as nausea, vomiting, indigestion, or stomach pain during a heart attack. These symptoms are sometimes mistaken for indigestion or other digestive issues.
- Dizziness or lightheadedness: Feeling lightheaded, dizzy, or experiencing unexplained episodes of fainting can be a symptom of heart disease in women.
- Sleep disturbances: Women with heart disease may experience sleep disturbances, including insomnia, restlessness, or excessive sweating during sleep.
It’s important to note that not all women will experience these symptoms, and the presence of these symptoms does not necessarily indicate heart disease. Women can also have atypical or “silent” heart attacks with minimal or no symptoms. If you have concerns about heart disease or experience any of these symptoms, it’s important to consult with a healthcare professional for proper evaluation and diagnosis.
What are the symptoms of heart disease in women?
Heart disease can have multiple causes, and it often results from a combination of factors. Here are some common causes and risk factors associated with the development of heart disease:
- Atherosclerosis: The primary cause of coronary artery disease (CAD), atherosclerosis occurs when fatty deposits called plaque build up inside the arteries. Plaque narrows the arteries, reducing blood flow to the heart and increasing the risk of heart disease.
- High blood pressure (hypertension): Elevated blood pressure puts strain on the heart and blood vessels, leading to their damage over time. Hypertension is a significant risk factor for heart disease, including heart attacks, heart failure, and stroke.
- High cholesterol: Elevated levels of LDL (bad) cholesterol and triglycerides in the blood contribute to the development of plaque in the arteries, leading to atherosclerosis and increasing the risk of heart disease.
- Smoking: Cigarette smoking damages the blood vessels, reduces oxygen supply, raises blood pressure, and increases the risk of atherosclerosis and blood clot formation, making it a significant risk factor for heart disease.
- Diabetes: Individuals with diabetes have a higher risk of developing heart disease. Poorly controlled blood sugar levels can damage blood vessels and nerves, increasing the likelihood of atherosclerosis.
- Obesity and sedentary lifestyle: Excess weight and a sedentary lifestyle contribute to the development of heart disease. They increase the risk of high blood pressure, high cholesterol, type 2 diabetes, and atherosclerosis.
- Family history and genetics: Having a family history of heart disease, especially at a young age, can increase an individual’s risk. Certain genetic factors and inherited conditions can also contribute to the development of heart disease.
- Age and gender: The risk of heart disease increases with age. Men are generally at higher risk of heart disease than premenopausal women. However, after menopause, women’s risk catches up to that of men.
- Poor diet: A diet high in saturated and trans fats, cholesterol, sodium, and added sugars can contribute to the development of heart disease. Lack of fruits, vegetables, whole grains, and fiber also increases the risk.
- Stress and mental health: Chronic stress, anxiety, and depression can have negative effects on heart health. They can contribute to high blood pressure, unhealthy coping behaviors (such as overeating or smoking), and an increased risk of heart disease.
It’s important to note that while these factors increase the risk of heart disease, they do not guarantee its development. Adopting a healthy lifestyle, managing risk factors, and seeking regular medical check-ups are crucial for preventing or managing heart disease.
What are some risk factors for heart disease?
There are several risk factors associated with an increased likelihood of developing heart disease. These risk factors can be categorized as modifiable and non-modifiable. Modifiable risk factors can be changed or controlled through lifestyle modifications or medical interventions, while non-modifiable risk factors cannot be changed. Here are some common risk factors for heart disease:
- Modifiable Risk Factors:
- High blood pressure (hypertension)
- High cholesterol levels (especially elevated LDL cholesterol and triglycerides)
- Smoking or exposure to secondhand smoke
- Diabetes or high blood sugar levels
- Obesity or being overweight, particularly excess abdominal fat
- Sedentary lifestyle and lack of regular physical activity
- Unhealthy diet high in saturated and trans fats, cholesterol, and sodium, and low in fruits, vegetables, whole grains, and fiber
- Excessive alcohol consumption
- Stress, anxiety, and depression
- Sleep apnea and poor sleep quality
- Non-Modifiable Risk Factors:
- Age: The risk of heart disease increases with age.
- Gender: Men have a higher risk of heart disease than premenopausal women. However, women’s risk catches up to that of men after menopause.
- Family history: Having a close family member (such as a parent or sibling) with a history of heart disease increases the risk.
- Ethnicity: Certain ethnic groups, such as African Americans, Hispanics, and South Asians, have a higher risk of heart disease.
- Genetic factors: Certain genetic conditions or inherited traits can increase the risk of heart disease.
It’s important to note that having one or more risk factors does not guarantee the development of heart disease. However, having multiple risk factors or a combination of modifiable and non-modifiable risk factors can significantly increase the likelihood of developing heart disease. It’s crucial to identify and manage these risk factors through lifestyle changes, medical interventions, and regular check-ups with a healthcare professional to reduce the risk of heart disease.
What treatments are available for heart disease?
The treatment options for heart disease depend on the specific condition and its severity. Here are some common treatments:
- Lifestyle changes: Making healthy lifestyle modifications can help manage and prevent heart disease. This includes adopting a balanced diet low in saturated and trans fats, engaging in regular physical activity, maintaining a healthy weight, quitting smoking, and managing stress levels.
- Medications: Several medications are used to treat heart disease, including:
- Statins: These drugs help lower cholesterol levels.
- Beta-blockers: They reduce blood pressure and heart rate, easing the workload on the heart.
- ACE inhibitors or ARBs: These medications lower blood pressure and can protect the heart.
- Antiplatelet drugs: Examples include aspirin and clopidogrel, which help prevent blood clots.
- Anticoagulants: Medications like warfarin or newer oral anticoagulants are used to prevent blood clots.
- Diuretics: These drugs help reduce fluid buildup and lower blood pressure.
- Procedures and surgeries: In more severe cases, invasive procedures or surgeries may be necessary. Some common interventions include:
- Angioplasty and stenting: A catheter with a balloon is used to open blocked or narrowed arteries, and a stent is placed to keep the artery open.
- Coronary artery bypass grafting (CABG): A surgical procedure that creates new pathways for blood flow by bypassing blocked or narrowed arteries using blood vessels from other parts of the body.
- Heart valve repair or replacement: Damaged or diseased heart valves may need surgical repair or replacement.
- Implantable devices: Devices like pacemakers, implantable cardioverter-defibrillators (ICDs), or cardiac resynchronization therapy (CRT) devices can help regulate heart rhythm and improve heart function.
- Cardiac rehabilitation: This comprehensive program combines exercise, education, and counseling to help individuals recover from heart-related procedures or manage their heart condition.
It’s important to note that the specific treatment plan will vary for each individual based on their unique circumstances. It is crucial to consult with a healthcare professional who can assess your condition and recommend the most appropriate treatments for you.

Leave a comment